Payer Requirement Settings
This section describes what happens when you set a specific requirement for a plan or policy.
If you are looking for information on how to add or modify an insurance payer, go here.
-
During claim creation, the ET modifier is auto-populated to charges where the "Patient was transported in an emergency situation" is selected in the Patient Details tab.
-
The ET modifier will be placed in the first position.
-
For primary payers, if the claim does not have the ET modifier, a warning message displays: "XX requires the ET modifier be included on this claim's charges. To include it in the submission, update the claim's charges to include ET in the first position."
In some areas of the country, Medicaid will pay more if the trip originated from a rural or super-rural area. In order to get this increased rate you must apply a TN modifier to the charges section of the claim.
-
A TN modifier is auto-populated to the claim's charges when there is a rural or super-rural pickup location.
-
The modifier will be applied to the last position.
-
This rule apples to the primary and secondary payer. The TN modifier is applied to the claim's charges when the claim moves to a secondary payer that has this requirement set.
-
This setting applies to new claims and those updated claims that include payers with this requirement.
-
A U1/U2 modifier will be auto-populated to the claim's ground mileage (AO425) charges.
-
U1 will be applied to everything in ALS that is not covered in BLS.
-
U2 will be applied for BLS. Level of service for BLS includes BLS non-emergency, BLS emergency, service car, and unlisted ambulance service.
-
U1/U2 modifiers do not apply to non-emergency-stretcher, fixed and rotary wing, and wheelchair.
-
The modifier will be placed in the first position.
Implement this requirement at the policy and benefit level to merge mileage charges exceeding 999 into a single charge line. When activated, mileage charges with a quantity greater than 999 in section 24 of the CMS 1500 form will not be divided. If the mileage exceeds 100, it will be rounded up to the nearest whole mile.
-
When set, the "Include emergency indicator in submission" checkbox will be auto-selected during claim creation.
-
If the checkbox is not selected, then a warning message displays.
-
An emergency claim is identified when the transport type "Patient was transported in an emergency situation" was selected.
When this requirement is enabled, claims must have a place of service other than 41 or 42 before they can be submitted.
If the place of service is 41 or 42 when you try to submit the claim, a message will display that reads, "Place of service 41 and 42 are not valid for current payer. To edit the place of service, navitagate to the Incident Details tab."
There will be an audit trail entry when a user changes the place of service from XXX to XXX.
-
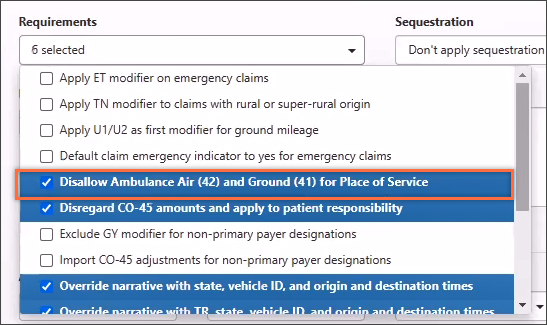
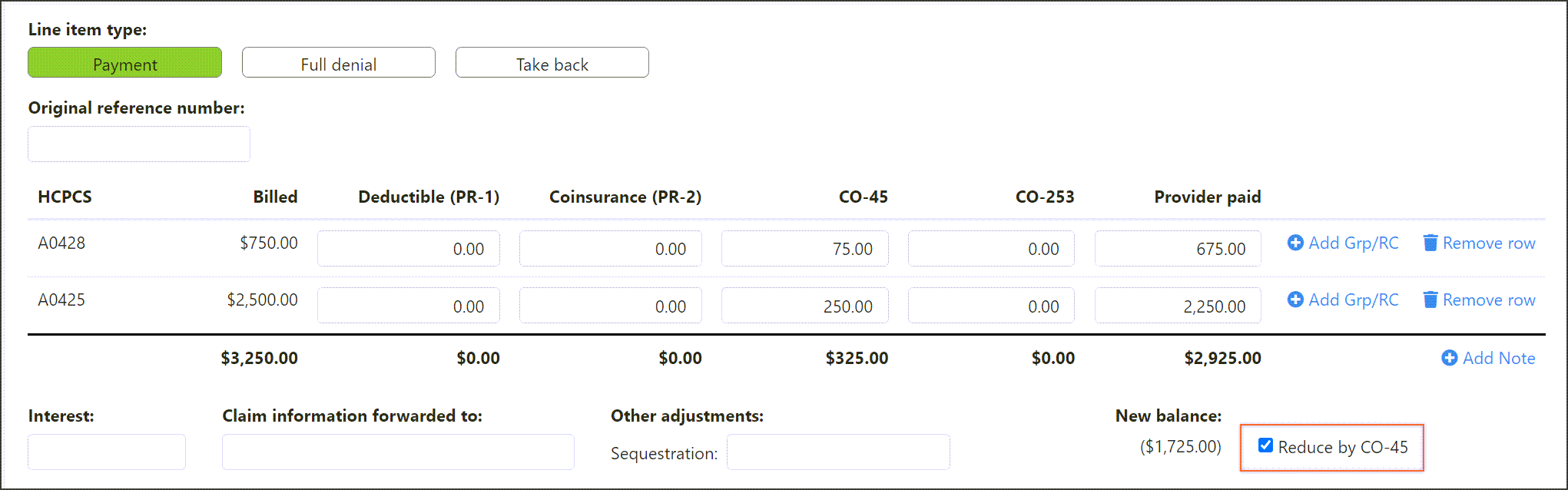
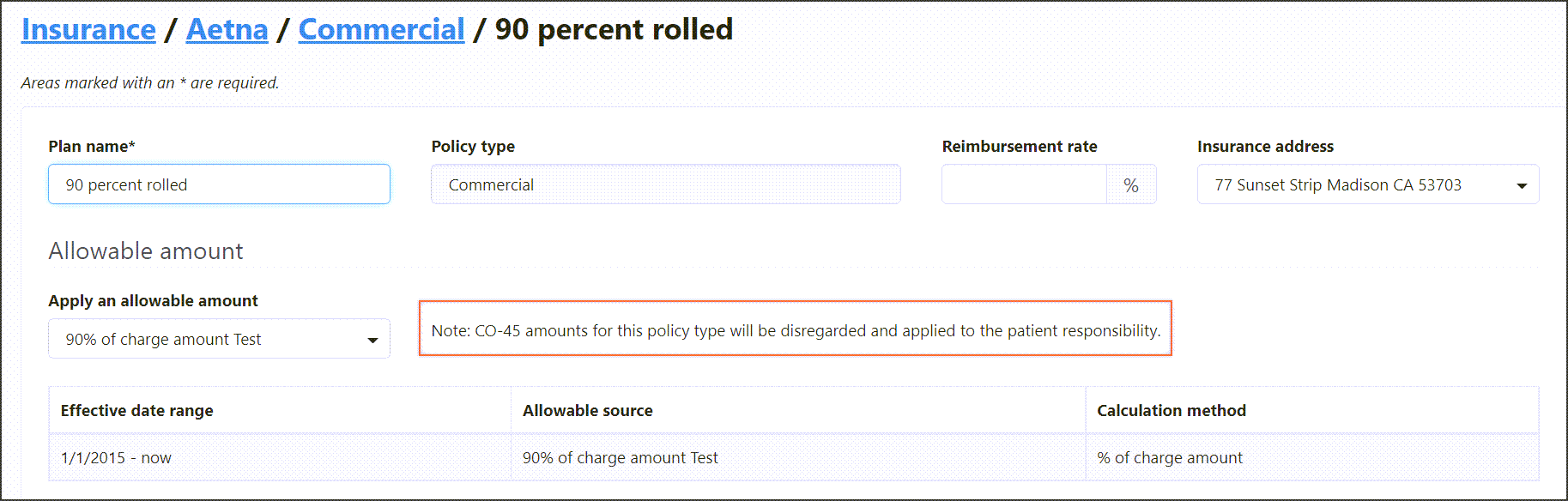
Controls the 'Reduced by CO-45' option on the Payment Posting page.
-
When set in Admin, a note will display on the policy level of an insurance.
-
This rule overrides the claim's narrative field with the state, vehicle ID, and original and destination times.
-
The rule is applied during claim creation or when you update the COB with a payer that has this requirement set.
The auto-fill narrative requirement in Admin > Insurance > policy & benefit automatically enters a specific text description to the narrative field on the "Level of service & diagnosis" tab.
When this requirement is set, the narrative displays as follows:
Origin State, Vehicle ID (8-characters – if the vehicle ID is less than 8-characters you will see spaces at the end), Origin Time (HHMM format), Destination Time (HHMM format)
Example: IL,12345678,1155,1220
This narrative overrides any narrative that exists in the Narrative field.
To enable this requirement:
-
On the navigation bar, click Admin.
-
Click the Billing tile.
-
Click the Insurance tile.
-
Select your insurance from the list and then select the policy or benefit plan.
Important!
-
If you enable a requirement at the policy level, that setting is automatically set for every benefit plan under it. You cannot disable a requirement on the benefit plan that is set at the policy level.
-
However, you can enable additional requirements on the benefit plan that is not set on the policy.
-
-
On the policy or benefit plan, click the Requirements field and select Override narrative with TR, state, vehicle ID, and origin and destination times.
-
Click Save.
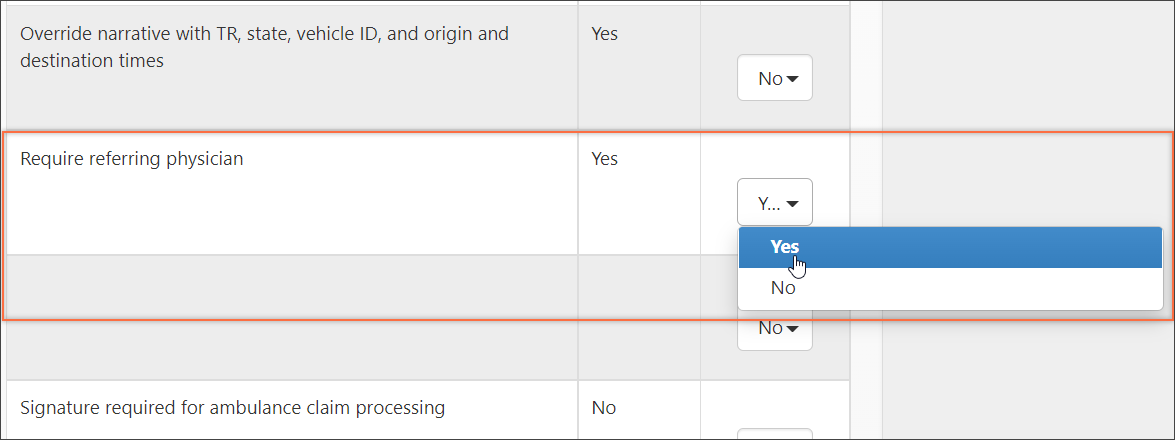
To ensure that a referring physician displays on all claims for a given insurance, we created a new payer level requirement at both the policy and plan level. If set, a referring physician will be required for that payer no matter where it exists in the coordination of benefits (primary/secondary/tertiary).
Policy
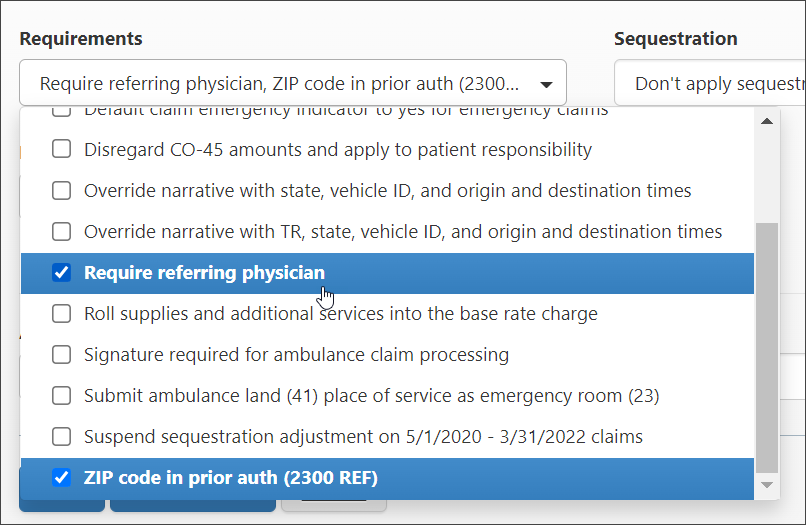
Plan
Required fields
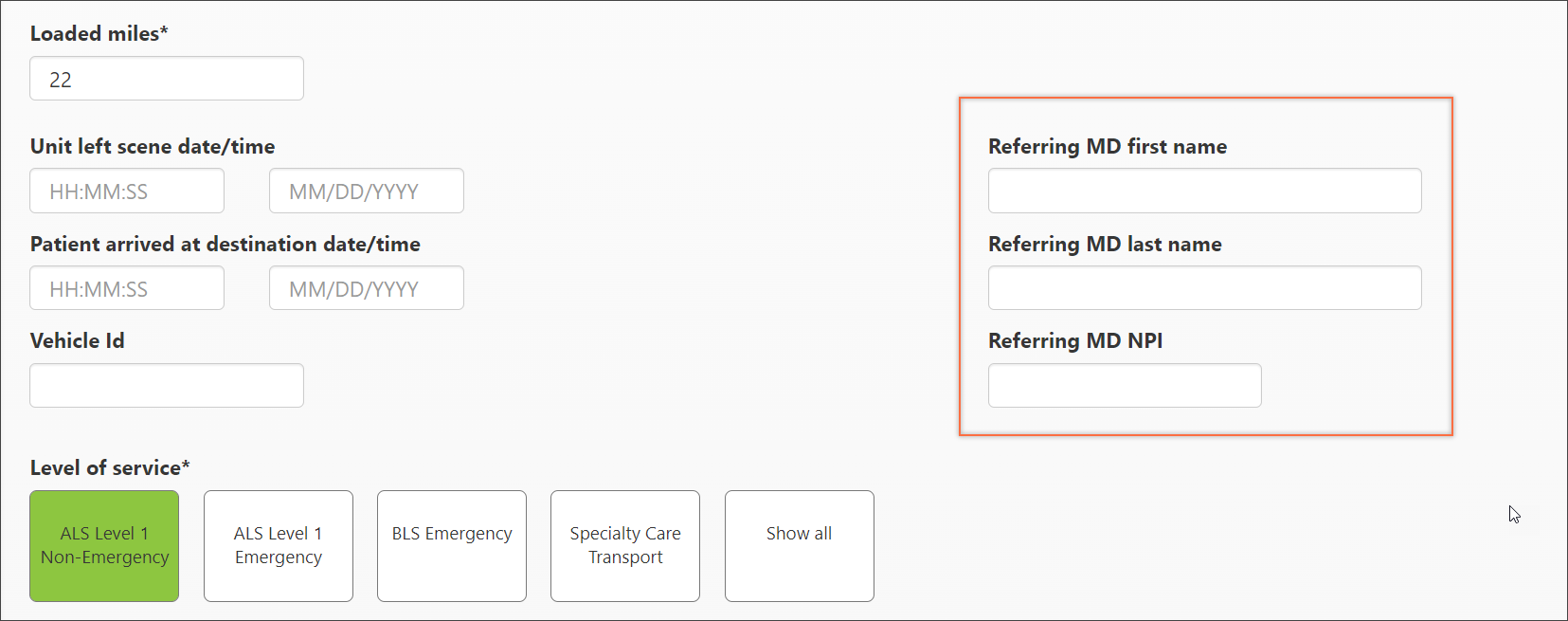
If the "Require referring physician" requirement is set, the following Incident details fields must be filled out when selecting this payer:
-
Referring MD last name
-
Referring MD NPI
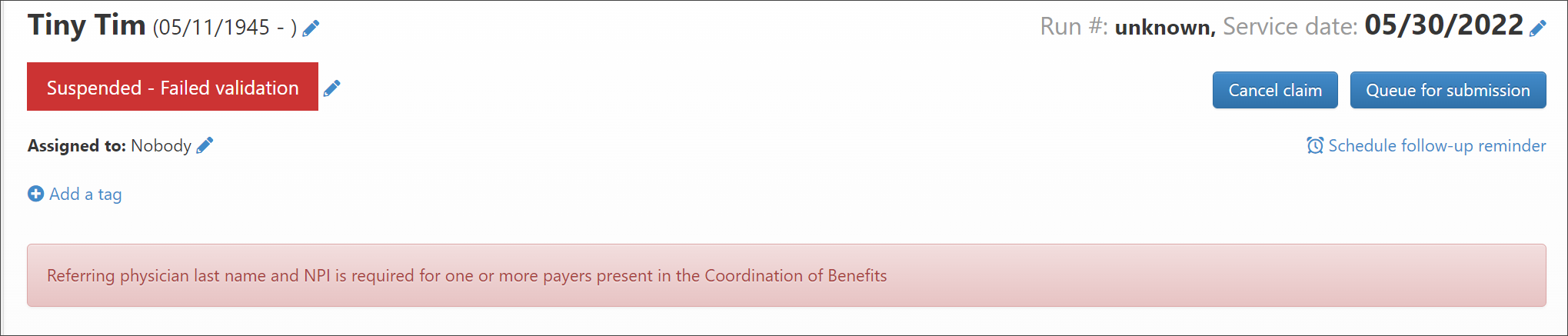
If they are not filled out, the claim will fail validation when submitted and you will see this error.
-
This setting will roll the supplies and additional charges into the base rate charge.
-
A signature must be applied to the claim before it can be submitted.
-
A validation message will display on the Claim page if a signature is not applied to the claim.
-
Instead of the ambulance land code '41', the emergency room code '23' is output on the 1500 form, box 24b (place for the service code).
-
When this rule is applied, sequestration is bypassed on claims with dates from 5/1/2020 - 3/31/2022.
-
Instead of the prior authorization number, pickup ZIP code will be outputted on the 1500 form in box 23 (prior authorization number).
-
Allows contractual allowances to import and process non-primary payments for non-primary payer policy/plans.
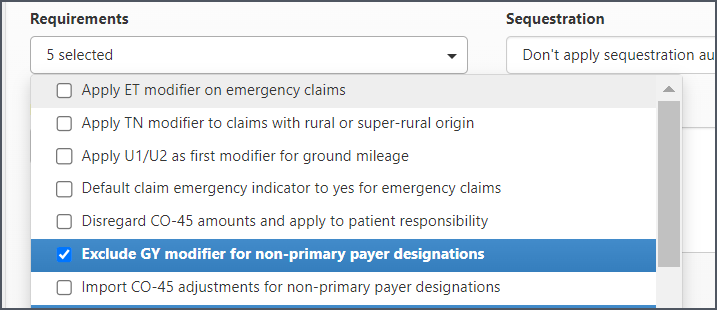
When this requirement is enabled on either the policy or plan level, the GY modifier will not go out on non-primary claims.
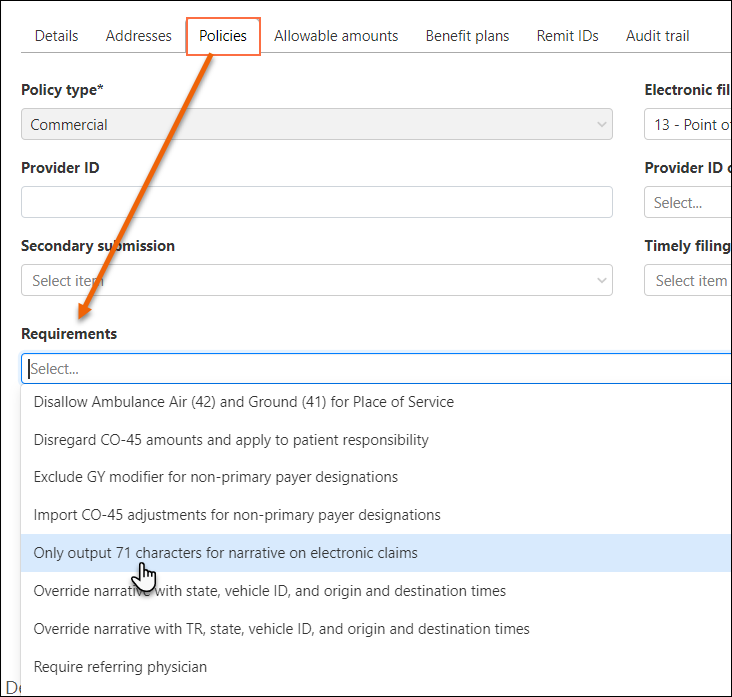
Set this payer requirement on the Policy and Benefit plan level to truncate the narrative on electronic claims to output 71 characters only. This requirement will default to NO.
Set the requirement at the benefit plan level
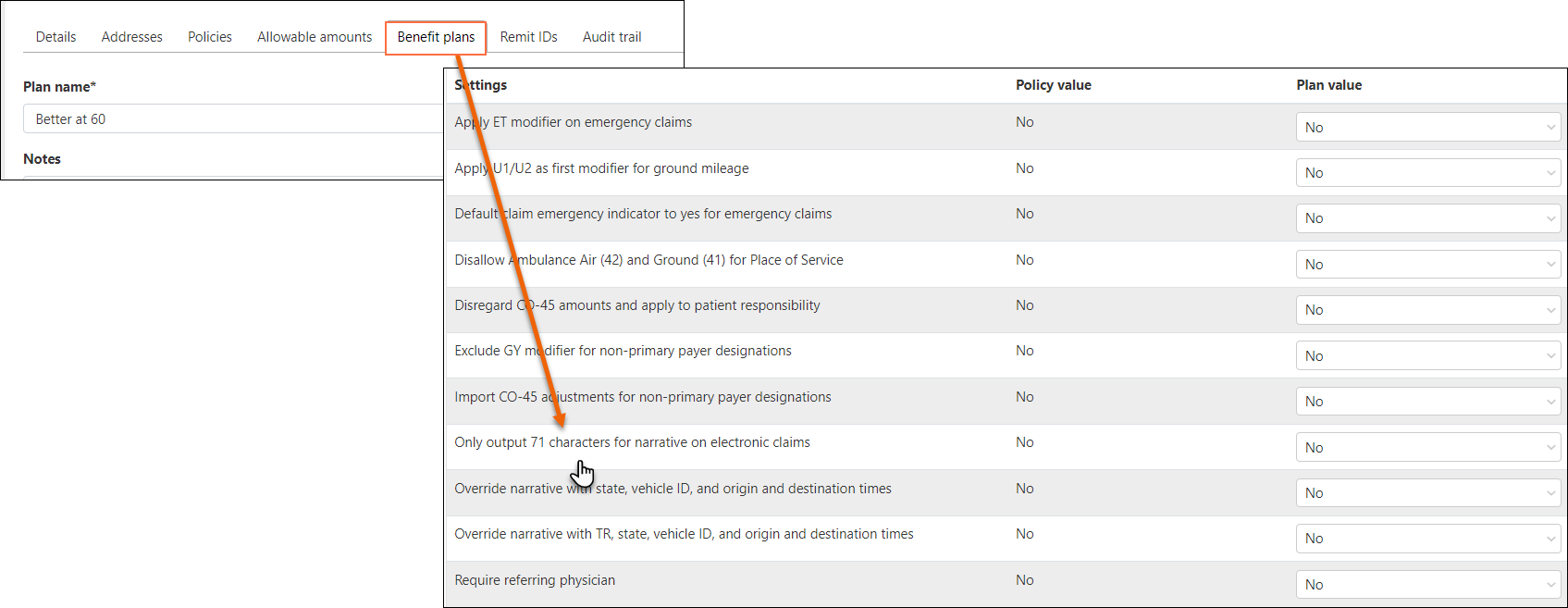
Set the requirement at the Policy level